Suicidality is a prevalent and complex problem in society today. As September is Suicide Awareness Month, it seems timely to revisit DBT’s approach to this global issue. In DBT, we try to understand what emotions are driving a client to suicide while also motivating clients to choose behaviors that fall in line with a life that is worth living. Oftentimes a client doesn’t necessarily want to die, rather they are in immense emotional pain and do not have the skills to ameliorate their intense emotions and pervasive thoughts. The model of comprehensive DBT, which will be detailed in this article, has been proven to effectively decrease the likelihood of ongoing behaviors. DBT’s approach focuses on preventing suicide while creating a “life worth living.” Thus, the objective is to enhance life instead of shielding the client from their pain, which is what suicidal behaviors aim to do.
The Biosocial Theory
It can be extremely difficult for loved ones to fathom how their friend/family member came to such a desperate place, and often loved ones do not know how to validate the pain they are experiencing for fear that this could lead to increased suicidal or self-harming behavior. It is crucial to understand DBT’s biosocial theory, the importance of validation, and how to invalidate the invalid. For instance, you might say, “it is completely understandable that you are feeling miserable in this situation and suicide is not the answer.” DBT’s biosocial theory posits that it is a transaction between innate emotional sensitivity and an invalidating environment that leads to emotion dysregulation and an inability to tolerate extreme distress, resulting in suicidal and self-injurious behaviors. Emotional sensitivity is characterized by high sensitivity, reactivity, and/or a slow return to baseline. Invalidation occurs when a person’s environment communicates, either directly or indirectly, that their private emotional experiences or expressions are “wrong.” While the term “invalidating environment” conjures up images of abuse and overt cruelty, this is often not the case. Many invalidating environments take the form of discouraging “negative” emotions or oversimplifying problem solving. For instance, if a child is crying, their caregiver might say something to the effect of “Why are you crying? There’s nothing to cry about” or “If you could finish your schoolwork on time, you wouldn’t be in this position.” These invalidating statements tend to affect people who have a high level of emotional sensitivity far more than those without a sensitive temperament. Thus, the emotionally vulnerable person becomes reactive, trying to prove that their emotions are in fact valid, which then escalates the invalidation from their environment and the transaction continues.
DBT’s View on Hospitalization
Many clinicians will choose to hospitalize their suicidal client as a means to keep the client safe. While this intervention may be effective in certain contexts, it is not always. DBT’s approach and stance on hospitalization is quite different from that of other therapeutic modalities. DBT routinely uses outpatient treatment in order to navigate suicidality and increase life satisfaction. While hospitals serve as good holding cells, preventing clients from harming themselves, there is no evidence that hospitalization decreases chronic suicidality any more than outpatient treatment does. In fact, there is some evidence to support the theory that hospitalization may actually have iatrogenic effects on suicidality. Data shows that not only is suicide the leading cause of death on inpatient psychiatric units, but that clients are at highest risk for completing suicide in the week to year following release from an inpatient facility. Additionally, DBT clinicians believe that hospitalization inadvertently reinforces suicidal behaviors, as clients learn that they will be contained and nurtured following a suicide attempt or self-injurious behavior, in essence, validating the behavior. While there are some exceptions, it is for these reasons that DBT therapists steer clear of hospitalization whenever possible.
A Life Worth Living Program
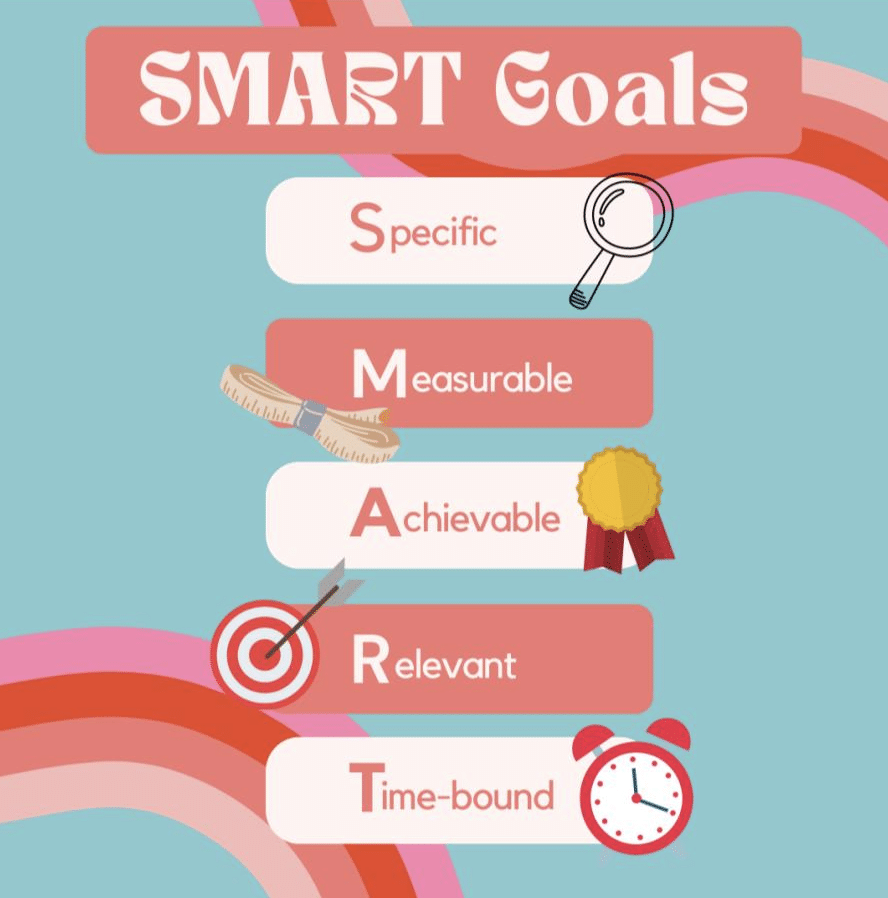
The primary focus of DBT is to help the client create a life for themselves that they feel is worth staying alive for. The individual clinician assists their client in creating a “life worth living” by first looking at their values in order to determine goals for their lives. Once the client has set some short and long-term goals, the clinician guides them through the process of breaking down goals into action steps which are specific, measurable, achievable, relevant, and time-bound (otherwise known as SMART goals- see fig. below). As the client progresses in their recovery and they begin to achieve their set goals, they become more motivated to continue their lives in a way that feels meaningful to them.
The Treatment
The comprehensive model of DBT includes five components (see fig. below). The components of DBT are as follows: Individual psychotherapy, skills training, phone coaching, clinician consultation team, and case management (as needed). Each component serves a function that helps to relieve chronic suicidality and increase the possibility of creating a valued life. Weekly individual therapy aids to increase clients’ motivation and decrease maladaptive behaviors. Skills training, usually executed in a group format, addresses clients’ skills deficits and enhances capabilities in the areas of mindfulness, distress tolerance, emotion regulation and interpersonal effectiveness. Phone coaching, in which DBT clients are able to contact their individual therapist for skill strengthening and generalization, ensures that the skills learned during group are generalized to all contexts of the client’s life. Case management, when needed, functions to psycho-educate and to structure the client’s often chaotic environment. Finally, the DBT consultation team is a weekly meeting in which individual clinicians enhance their own motivation and capabilities in order to best serve their clients.
If you or a loved one is experiencing suicidal behaviors and/or non-suicidal self-injury, there is a solution. DBT is an evidence-based treatment to address these very behaviors. DBT clinicians strive to be non-judgmental in their approach while balancing acceptance and change-based strategies. They teach this balance to their clients, encouraging them to find a middle path between accepting the reality of their lives and their pain while pushing themselves to change what they can control in order to make their lives worth living.